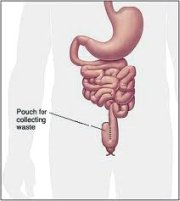
Pouchitis affects those, typically with ulcerative colitis, who have undergone ileal pouch-anal anastomosis (also known as j-pouch surgery), to create a surgical alternative to the colon. Pouchitis occurs when this surgically created pouch, known as an ileal-anal pouch or J-pouch, becomes inflamed. This condition affects approximately thirty-two percent of patients with an ileoanal pouch. The longer the time since the pouch was created, the greater the likelihood of the pouch becoming inflamed. The symptoms include:
- Bloody diarrhea
- More frequent bowel movements
- Discomfort in passing stools
- Cramping abdominal pain
- Fever
Pouchitis Treatment
The condition is usually treated with antibiotics. Immunosuppressant drugs may also be used.
That antibiotics prove useful in treating this condition indicates that bacteria are likely to play a role in pouchitis.
Evidence from clinical experience also supports this theory, concluding that the disorder “appears to be associated with high concentrations of bacteria”1.
Additionally, sufferers have been shown to have decreased levels of the beneficial bacteria lactobacilli and bifidobacteria in their colons, more of the less helpful bacteria Clostridium perfringens, as well as species such as fungi that were not found in controls2. As a result, the possible role of probiotics to restore bacterial balance and treat this disorder is receiving increased interest in the scientific community.
Evidence for Probiotics in the Treatment of Pouchitis
Although it must be said that research is in its early days, initial evidence for the use of probiotics in the treatment of ileal-anal pouch inflammation is promising. Numerous different probiotic formulations have been used in these studies. The probiotic supplement VSL3 and Lactobacillus rhamnosus GG, which is also marketed under the name Culturelle probiotic products, have proved to be useful in helping pouchitis patients.
The probiotic supplement VSL3 has been shown to be of benefit to pouchitis patients in two double-blind placebo controlled trials. In the first trial of thirty-six patients with recurrent or refractory pouchitis (i.e. that which does not respond to antibiotic treatment), sixteen received the probiotic supplement VSL3, whilst the remaining twenty took a placebo. Of the patients who took the probiotic supplement, 85% of sufferers had not experienced a relapse after one year of therapy compared to only 6% of those taking the placebo3.
In the second trial of twenty-three patients with mild, active pouchitis, 69% of those who took VSL3 for a four week period achieved remission4.
Several other research projects have used different probiotic species with pouchitis patients.
A trial using Lactobacillus rhamnosus GG (often marketed as Culturelle) indicated that this probiotic was useful if given immediately following initial j-pouch or ileal-anal pouch surgery. This trial concluded that therapy with between ten and twenty billion CFUs of Lactobacillus rhamnosus GG could delay the first onset of pouchitis for up to three years5.
Likewise a different scientific project using Lactobacillus acidophilus with Bifidobacterium lactis concluded that patients who consumed Cultura, a product containing these probiotics, over a four-week period, did show a decrease in their Pouchitis Disease Activity Index (PDAI) scores. These changed from a level considered to be diagnostic for pouchitis to one which is considered not active for pouchitis. The probiotic therapy however did not change either the mucosal inflammation of the pouch or the pouch blood flow6.
However a research trial using Lactobacillus rhamnosus GG for acute, active pouchitis did not show any therapeutic benefit from using probiotics, though the researchers did concede that the use of this probiotic had indeed positively influenced the pouch bacterial flora7.
Should I Try Probiotics for Pouchitis?
The study of probiotics for pouchitis is very new, but it does seem that probiotics may be useful in:
- Achieving remission after treatment with antibiotics.
- Delaying the onset of the initial bout of pouchitis.
There is, however, to date not enough evidence to suggest that probiotics are of use in treating acute, severe pouchitis – more research is needed into this aspect and indeed into the clinical use of probiotics for pouchitis in general. Future evidence, the existing data in this area as well as the growing body of evidence supporting the use of probiotics in ulcerative colitis, may indeed lead to more mainstream use of probiotics for pouchitis in the future.
In the meantime though, if you think from reading this page that probiotics could be of use in your situation, be sure to consult your physician before you begin. Ensure too that you take the same strains and quantities that have been proven to be of use for pouchitis.

